This blog post is different than my previous. As a medical student on rotations, I am constantly faced with a wide variety of events, some more dramatic than others. In the process, I research current literature and methods of treatment. The following is a recent encounter with a patient infected with tetanus. From history, I soon discover that despite being recently immunized with a booster shot, patient continued to display the classic presentation of tetanus, which unfortunately turned for the worse. In her remembrance and for a better cause, I put together a review on tetanus and what you have to know to prevent its infection. Know what you should do to prevent its manifestations. The story begins with a review.
If you thought you were immunized, think again...
Tetanus is an acute often fatal Nervous System (NS) disorder characterized by SUSTAINED muscle spasms and convulsions caused by the toxin-producing anaerobe CLOSTRIDIUM TETANI, which is a obligate anaerobe Gram+ Bacilli (exotoxin), typically found in soil.
Its clinical features and presentation associated with traumatic injuries have been well-known before the introduction of tetanus toxoid vaccination in 1940’s (among ancient Greeks and Egyptians).
This is the only vaccine preventible disease that is infectious but not contagious between humans.
Keep in mind that the typical bacteria forms a terminal spore that is resistant to heat and antiseptics. However, the organism outside the spore is very sensitive to Oxygen and heat. Another thing to keep in mind is the very low concentration of toxin needed - minimal lethal dose is 2.5 nanograms/Kg.
Clostridium Tetani usually enters the body through a deep penetrating wound. In presence of anaerobic conditions, typically seen with a local inflammation or early infection, the spores germinate, which later produce the bacteria and the toxin, disseminated via blood and lymphatics.
Toxin acts at certain CNS locations: peripheral motor end-plates, spinal cord, brain, and sympathetic nervous system. Toxin interferes with release of neurotransmitters, blocking inhibitor impulses, which leads to unopposed muscle contraction, and autonomic NS may also be affected.
Once Clinical manifestation occurs after tetanus reached the presynaptic inhibitory nerves, there is little that can be done to slow down disease progression. In assessing prognosis, generally the shorter the incubation the worse the outcome.
Incidence and mortality from tetanus by age group in the United States, 1998–2000. (From Pascual FB, et al: Tetanus surveillance—United States, 1998–2000. MMWR Surveill Summ 52[SS-3]:1, 2003.)
Despite the availability of an effective vaccine, tetanus remains endemic worldwide. It is more common in warm, damp climates and relatively rare in cold regions. The global incidence of tetanus is estimated to be between 800,000 and 1 million cases a year, with half occurring in neonates.
Since the introduction of vaccination programs in the United States, the incidence of tetanus has steadily declined from 4 cases per million population in the 1940s to 0.095 cases per million population in 2005.
The highest incidences occurs in people older than 60 years (0.35 cases per million population), Hispanic Americans (0.37 cases per million population), and diabetics (0.70 cases per million population). Fifteen percent of cases occur in injection drug users. The overall case fatality rate is 18% but approaches 50% in patients older than 70 years. Cases have been reported in patients who had been fully vaccinated, but in the eight patients from 1998 to 2000, no deaths occurred.
Clinical Diagnosis: Trismus
trismus |ˈtrizməs|nounMedicinespasm of the jaw muscles, causing the mouth to remain tightly closed, typically as a symptom of tetanus. Also called lockjaw.ORIGIN late 17th cent.: from modern Latin, from Greek trismos ‘a scream, grinding.’
Cultures (anaerobes, time consuming, takes minimum three days to get results back; half the time, the results are false negative because of the difficulty localizing and culturing the bacilli).
Differentials:
- Strychnine Poisoning Dystonic reactions to Dopamine Antagonist drugs
- Oropharyngeal infection (DDX Cephalic Tetanus)
- Hypocalcemia (DDX Neonatal Tetanus)
- Meningoencephalitis (DDX Neonatal Tetanus).
The goal of immunization is to provide a continuous serum concentration of 0.01 IU/mL of neutralizing antitoxin. Protection between levels of 0.01 and 1.0 IU/mL is not absolute; some authorities consider an antibody level of 0.15 IU/mL or greater as protective.
Active Immunization is achieved via the Tetanus Toxoid (takes time to build immunity).
Passive Immunization is achieved via the Immune Globulin TIG (passive transfer of active immunoglobulins).
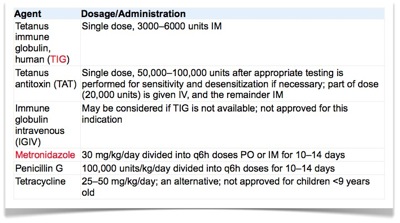
Immunization is given immediately if the patient's tetanus immunization history is not available or is uncertain, or if 60 months or more have elapsed since the last booster dose (5 years or more). TIG is given for other than minor wounds if the number of immunization doses the patient received is fewer than three or is unknown. The antibodies neutralize only free toxins, toxin not bound to nerve.
Table 1. Example of management pre-exposure, typically seen in pediatric patients:
Primary and Secondary Immunization.
Table 2. Example of management post-exposure:
The four treatment strategies for patients with tetanus should be undertaken simultaneously: (1) aggressive supportive care, control of muscle spasm with Benzodiazepines - most IV benzos except midazolam have propylene glycol as a coingredient which at high doses causes Lactic Acidosis. But midazolam has a short half life. (2) elimination of unbound TS (tetanospasmin), with HTIG or TIG (passive immunization) (3) active immunization, and (4) prevention of further toxin production - treating the C.tetani infection via wound debridement and ABX metronidazole.
Metronidazole - antibacterial, antiprotozoal, microbicidal, against most obligate anaerobics and protozoa, interferes with DNA/ Cytotoxic.
Penicillin - antibacterial, blocks cell wall synthesis, against gram+ bacteria and spirochetes.
Tetracycline - protein synthesis inhibition, bacteriostatic against both Gram+ and Gram -.
CASE PRESENTATION:
Chief Complaint (CC): This is the case of an 86yo female status-post (s/p) 1 day inability to open mouth, s/p 6 days rusty metal puncture wound Right Lower Extremity RLE.
NLDOCATS*: Patient (PT) complaints of generalized dull aching pain with a scale of 8-9/10 (0 no pain, 10 worst pain) to leg, neck, and abdomen. Pt relates to a 6 (SIX) days old puncture wound to lower extremity (LE) from a rusty metal soft tissue traumatic encounter. Pt relates to onset of fever and chills several days after her initial injury (day zero) for which she has taken Cipro orally prescribed by her primary care physician (PCP) over the phone. Pt relates, her fever resolved uneventfully. However, pt states few days later after taking Cipro orally, she was awaken to discover her inability to open mouth more than a few millimeters, along with increased stiffness to the neck muscles throughout the morning hours. In patient's defense, a confirmed recent Tetanus booster was completed mid-September 2011, prescribed by her PCP.
(*Nature, Location, Duration, Onset, Course, Aggravating factors, Treatment, Special)
Past medical, surgical, and social histories are non contributory.
Pt allergies are as follows: Aspirin, Penicillin, Sulfa, Ceclor, Mefoxin, Tetracycline, Nalidixic Acid (Neggram), all producing asthma-like reaction.
Current Medications: Prednisone 10mg QOD , Theophylline 100mg daily, Beclomethasone spray QID , Albuterol MDI 2 puffs QID , Imodium PRN, Primidone 50mg at bed time , Fish Oil , MVI, Vit-C, Ca, Vit-D.
Review of Systems: (ROS) Abdominal pain, Diffuse muscle stiffness, Puncture wound RLE with surrounding erythema, Bruising, ELSE remainder of ROS is non contributory
Physical Exam:
Vital Signs: T 96.8, HR 85, RR 16, BP 150/78, PO2 99% room air .
General: Awake Alert and Oriented to person, place, & time (AAOx3), Emaciated, Restless
HEENT: Atraumatic, Normocephalic Anicteric, External ocular movements intact, pupils equally round reactive to light and accommodation (PERRLA), Unable to open jaw > 0.5cm, mucous membrane moist, teeth worn
Neck: Post cervical neck muscles are spastic, tender ,
Cardiovascular: regular rate and rhythm (RRR), no murmurs, gallops, rubs, S3, S4, no peripheral edema
Respiratory: clear to auscultation (CTA) bilaterally (BIL), no wheezing, crackles
Abdomen: normative bowel sounds (BS), abdomen firm to palpation, unable to determine hepatoslenomegaly given muscle rigidity
Extremities: UE Strength 5/5 BIL, epicritic sensation intact in all 4 extremities, LE Strength 4/5 BIL, R-Knee Extension 2/5, Dorsal Plantar flexion 5/5 BIL. There is 1-1.5cm circular area of necrosis on Lat LE with fresh tissue in middle that is leaking clear fluid, surrounding erythema cold to palpation, nontender to palpation.
Neurologic: Cranial nerves II-XII intact, when asked to smile patient exhibited sardonic smile, baseline tremor in BIL hands. Muscle strength as described above. Sensation intact to all 4 extremities
Psychiatric: AAOx3, fluent speech pattern, thoughts are logical, judgement and insight appear to be fair.
Laboratories: CBC & BMP are within normal limits
Podiatry Physical Exam: LE exam reveal several scabs and a wound on the L anterior leg. There are bandages, which are dry and intact and remain in place over this area. Left leg shows no erythema, edema, or heat. Pedal Pulses are palpable. Right leg exhibits significant erythema from the level of the mid calf distally. There is +1 pitting edema throughout the lower leg and foot. Pedal pulses palpable, however faint secondary to edema which is present. There is a dry bandage covering the wound located to the R lateral lower leg midtibia level. Examination of wound reveals a black eschar approximately 2cm diameter. Wound borders appear intact with notable erythema, edema, and heat throughout surrounding area. Noted induration palpable proximally and posteriorly to the wound, extending 3cm posteriorly. Upon compression of periwound area there is noted purulent fluid drainage from wound. Patient also responds and is sensitive to this palpation, attempting to retract leg.
Assessment & Plan:
1. Trismus with generalized spasticity consistent with Tetany. Give a total of 3000 Units IG. Start Metronidazole 500mg Q6H. Cardiac Monitoring. IV Fluids and Valium 2mg every 6h for muscle spasms. Also Magnesium sulfate IV 40mg/kg, or Labetalol IV 0.25-1.0mg per minute for autonomic dysfunction.
2. Nutrition, emaciated, NG tube or PEG placement for expected 4-6 weeks long tetany course
Podiatry Surgical Debridement:
Upon Examination, wound appeared erythematous with central eschar. Sharp debridement performed of all devitalized soft tissue, minimal purulence observed for which aerobic / anaerobic cultures were performed. Skin appeared atrophic dissecting easily along the superficial and deep fascial planes proximally. Mechanical Pulse-Lavage performed with 3000 mL Triple Antibiotic in sterile Normal Saline. Wound was packed open and sterile soft dressing applied. Patient transported to Recovery in stable condition, no complications observed.
Summary of Events:
Day 0: Injury
Day 4: Fever 100F, Sweats. Tx Cipro PO at home
Day 5: Symptoms resolve
Day 6: Locked Jaw, Stiff Neck, RLQ Pain, RLE Pain ➡ ED admission, Intubation, Tetanus IG 3000 IU, Metronidazole 500mg IV Q6H, Valium, IV fluids, Magnesium IV, Labetalol IV.
Day 7: Sx Wound Debridement w/ Pulse Lavage
Day 10: Severe generalized deterioration, Cardiovascular Instability, not responding to treatment, Autonomic NS failure, possibly Phrenic Nerve involvement.
Day 12: Immediate family disconnects life support, Pt expires within minutes.
RESOURCE - Tetanus Algorithm:
REFERENCES
1. C. Louise Thwaites, Lam Minh Yen, Harrison's Principles of
Internal Medicine, 18e, Infectious Diseases > Section 5. Diseases Caused by Gram-Positive Bacteria > Chapter 140. Tetanus, McGraw-Hill Companies 2012
2. Madonna Fernández-Frackelton, Infectious Diseases - Bacteria, Rosen's Emergency Medicine 7th Ed 2010
3. Itzhak Brook, Etiologic Agents of Infectious Diseases - Tetanus, Principles and practice of Pediatric Infections 3rd Ed, Churchill Livingstone, An Imprint of Elsevier, 2009
4. Pavani Reddy, Thomas P. Bleck, Clostridium tetani (Tetanus) 244, Bleck, Mandell, Douglas, & Bennett's Principles and Practice of Infectious Diseases, 7th ed - Textbook of Critical Care , Sixth Edition, 2009 - Churchill Livingstone, An Imprint of Elsevier
5. C. Louise Thwaites, Lam M. Yen, Tetanus 147, Bleck, Mandell, Douglas, & Bennett's Principles and Practice of Infectious Diseases, 7th ed - Textbook of Critical Care , Sixth Edition, 2009 - Churchill Livingstone, An Imprint of Elsevier
6. Gregory J. Moran et al, Antimicrobial Prophylaxis for Wounds and Procedures in the Emergency Department, Journal of Infectious Disease Clinics of North America, 22 (2008) 117–143
7. Basic Tetanus Algorithm, AJM PRiSM 2009
A LEARNING LESSON:
- if you suspect a dirty tetanus prone infection/deep skin cut
- flush the wound with clean water by placing the wound under running water, removing visible dirt, debris, or foreign materials; I recommend prying open the sound if it's large enough to ensure water flushing is maximized.
- do not apply sodium peroxide as this strong base will start the local inflammatory process secondary to complete cellular destruction, especially host skin and soft tissue; applying an antibiotic ointment is also not recommended since you need to keep the wound clean and dry for the time being.
- recall, tetanus spores do not like oxygen & dry environment
- apply a clean gauze / dressing over the affected area and have someone drive you to the nearest Emergency Department. The sterile gauze is the best method to keep the wound as dry as possible absorbing any serous or blood discharge from the wound preventing anaerobic environment.
- an injection of Immune Globulin is highly indicated despite your history of tetanus booster shots. Tetanus Immune Globulin (TIG) is the only known neutralizer of free unbound tetanus toxin that will soon be released from within the wound.
- a treatment of oral Metronidazole antibiotic (anti anaerobe gram positive bugs) is highly recommended to treat local soft tissue infection that might reverse the wound to an anaerobic environment.
- recall, the tetanus spore will germinate and release the bacilli into the wound as soon as the wound becomes anaerobic environment seen with early inflammation and infection. Once bacilli is aware of anaerobic environment it will quickly release its toxin which will travel via lymphatics and blood vessels selectively to nerves of muscle, spinal cord, and brain. Once toxin is bound to the nerve it will not be unbound until the nerve end-plate regrows a working duplicate bud that will replace the damaged end-plate - an approximate 4-6 weeks period.